Naloxone Toolkit
Overdose deaths remain at historically high levels in the United States. The Centers for Disease Control and Prevention (CDC) estimates that more than 107,543 people died from overdose in 2023.[1] Most of these deaths involved opioids. With the increased use of illicitly manufactured drugs such as fentanyl and xylazine as an adulterant to opioids, cocaine, methamphetamines, and others, the illicit drug supply has become increasingly lethal and unpredictable.[2] Given these realities, it is important that everyone has access to accurate and timely information about overdose risk and prevention. Evidence-based harm reduction strategies are available—knowing when and how to use them can help end the overdose crisis. This toolkit, focused on naloxone as one intervention, provides justice practitioners with the knowledge and tools needed to reduce opioid overdoses and help save lives.
The term “harm reduction” broadly refers to strategies that address and try to prevent the negative effects of substance use when people who use substances are not ready or able to stop use. Evidence shows that harm reduction strategies, such as naloxone, are effective in reducing overdose death, increasing referrals to treatment, and reducing infectious disease transmission. Recovery from substance use is not a straight line. Relapse can be a part of the recovery process, and harm reduction complements the delivery of evidence-based treatment and recovery support services.
-
Opioid overdose reversal medications (OORMs) are lifesaving medications that reverse the effects of an acute opioid overdose and restore breathing.
-
It is important to know the signs of an opioid overdose to act quickly and save a life.
-
An important part of the continuum of care for overdose response and prevention is providing follow-up to individuals who have overdosed and their families.
-
As of March 2023, naloxone, a safe, FDA-approved medication that has been proven to reverse opioid overdoses in minutes, is available without a prescription.
-
A variety of training and technical assistance is available to assist practitioners with developing a naloxone program in their communities as well as other evidence-based strategies for addressing the impact of substance use disorder.
-
Listing of promising practices through the United States.
FAQ
Approved by the FDA since the 1970s, naloxone is a very safe medication with the potential side effect of a theoretical risk of allergy that has never been documented. Its administration may result in acute opioid withdrawal (agitation, nausea, vomiting, diarrhea, "gooseflesh," tearing, runny nose, and yawning). When victims experience these symptoms, they may become irritable and anxious. It is uncommon, however, for a revived victim to become violent or combative. Intranasal naloxone delivery is less likely to result in severe withdrawal symptoms than an injection.
On rare occasions, reviving an opioid overdose victim may restart existing health problems or uncover the effect of other drugs the victim had taken. This may result in heart palpitations or seizures. In all cases of overdose, it is critical that victims be transferred to the care of medical professionals.
Naloxone is a fairly stable medication, with a shelf life between 18 months and 2 years. Intranasal and intramuscular naloxone should be stored between 59 and 86 degrees Fahrenheit and should be kept away from direct sunlight. In most law enforcement settings, naloxone can be stored in the cab of a vehicle. Alternatively, the medication has been stored with automated external defibrillator (AED) units.
A variety of resources are available to support the use of naloxone in the field. These resources are designed to help individuals and organizations implement effective overdose prevention and education programs and to provide guidance on the safe and effective use of naloxone in emergency situations.
One such resource is the Guide to Developing and Managing Overdose Prevention and Take-Home Naloxone Projects, which provides practical guidance on how to design and implement effective naloxone distribution programs. The guide includes information on key components of successful programs, such as identifying target populations, developing training protocols, and implementing quality assurance measures.
In addition, the CDC and SAMHSA National Harm Reduction Technical Assistance Center (NHRTAC) provide direct technical assistance to organizations seeking to develop and implement overdose prevention and education programs. This resource provides expert guidance on a variety of topics related to overdose prevention and naloxone distribution, including program design, training protocols, and quality assurance measures.
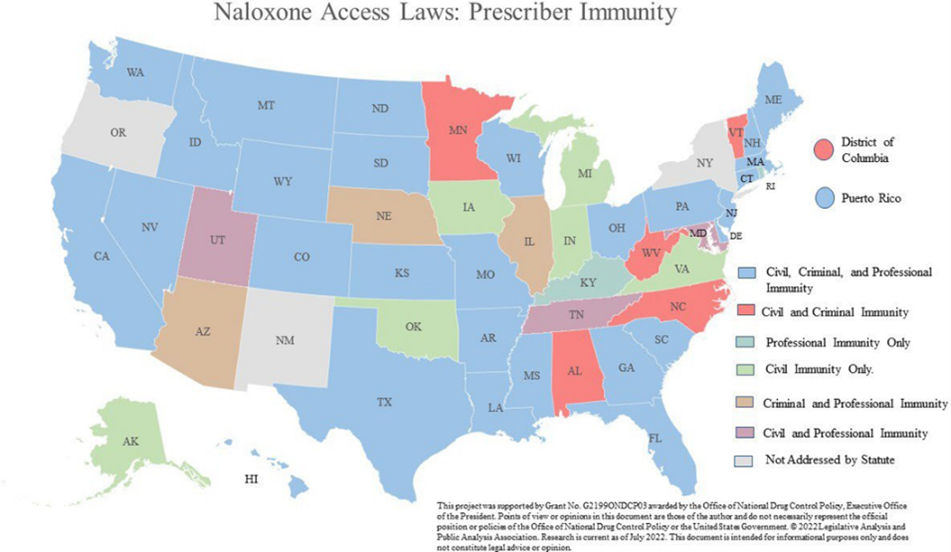
There are no federal restrictions on who may purchase nonprescription naloxone. Specific state laws vary.